Primary Care First (PCF) is a 5-year model aiming to improve quality, improve patient experience of care, and reduce expenditures. Clinical quality, utilization, and patient experience measures are used to assess quality of care delivered at the practice and PCF practice sites must meet standards that reflect quality care and model requirements in order to be eligible for a positive performance-based adjustment (PBA). The measures were selected to be actionable, clinically meaningful, and aligned with CMS’s broader quality measurement strategy.
The Patient Experience of Care Survey (PEC Survey), which is based on the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Clinician and Groups Survey (CG), is also required for all practice sites. Positive patient experience reflects high-quality care. Positive patient experience is also associated with higher levels of patient adherence, improved clinical outcomes, and lower utilization of inpatient and emergency department services. The designers of the PCF questionnaire specifically included CAHPS questions that measure whether patients observe providers and practice sites engaging in behaviors connected to PCF objectives, such as use of a care team with 24/7 access to the patient’s EHR and educating patients about how to get emergency care outside of practice hours.
CAHPS surveys are experience of care surveys, which are distinct from satisfaction surveys.
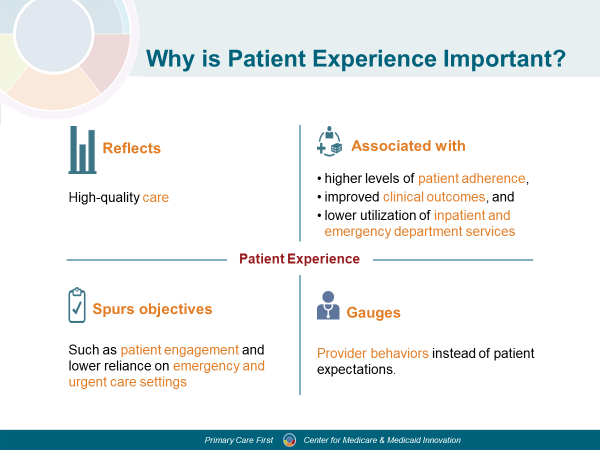
Why is Patient Experience important? CMS wants to ensure quality of care, especially the patient experience, is not negatively impacted in the alternative payment model used in PCF. Patient experience indicates high quality care has been provided. Positive patient experience is also associated with:
- higher levels of patient adherence,
- improved clinical outcomes, and
- lower utilization of inpatient and emergency department services.
Importantly, positive patient experience can be a lever to spur many objectives central to PCF, such as patient engagement and lower reliance on emergency and urgent care settings. Positive patient experience is associated with higher levels of patient adherence, improved clinical outcomes, and lower utilization of inpatient and emergency department services. For the practice, patient experience measures correlate with clinical care process measures that prevent and manage disease. Thus, positive patient experience reflects high-quality care.
Patient experience and patient satisfaction are not the same. Patient experience surveys ask patients specific, objective questions about the health care that occurred (whether it happened, how often it happened). By comparison, satisfaction surveys ask patients about their expectations and ratings of their health care, which can vary greatly by patient and are inherently subjective.
Roles and Responsibilities for the PCF PEC Survey
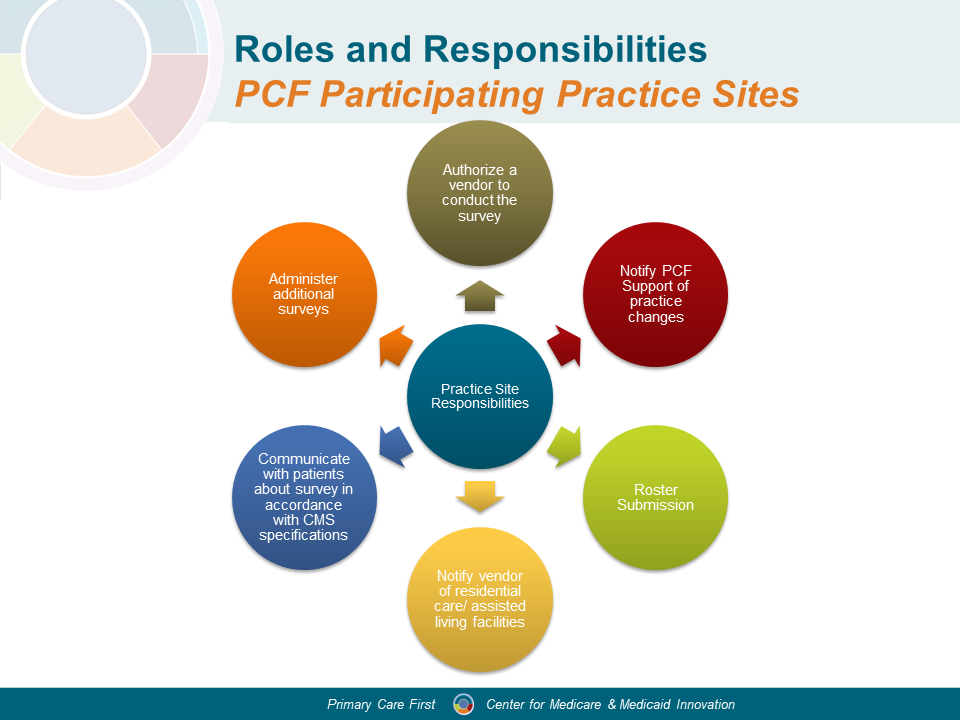
The PCF PEC Survey protocol follows the same model as other CAHPS surveys, such as the Home Health Care CAHPS (HHCAHPS) Survey, In-Center Hemodialysis CAHPS (ICH CAHPS), and Outpatient and Ambulatory Surgery (OAS CAHPS), where providers contract with approved survey vendors for the data collection and implementation of the survey. Practice Sites will receive a CMS-approved list of survey vendors no later than 120 days prior to the survey administration date. CMS has adopted standardized survey protocols that allow for varying survey costs and ensured that the approved vendors are trained to implement these protocols consistently. Like these other CAHPS surveys, the PCF PEC Survey will utilize a survey website as a centralized location for survey vendor resources, application, training, sample download, and data upload. Practice Sites will receive additional information about survey vendors via First Edition and Connect.
Schedule for the PCF PEC Survey
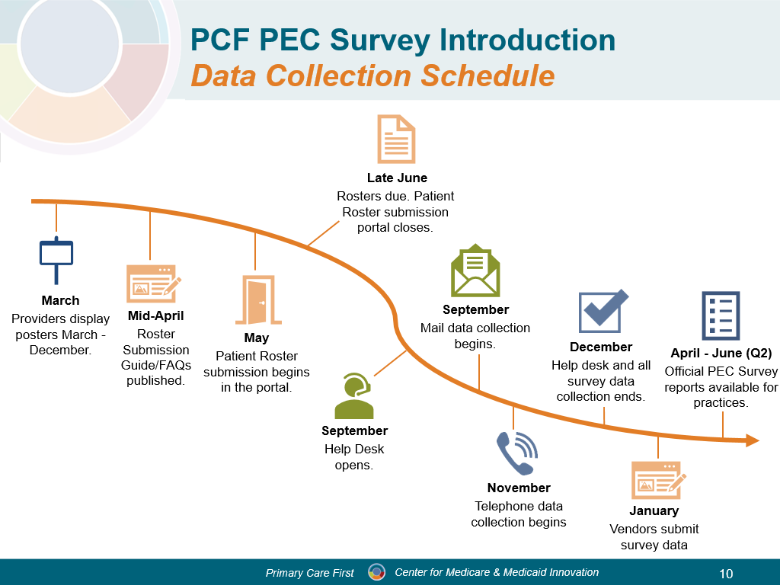
CMS asks that providers display PEC Survey posters April-December of each performance year. This will allow time for patients to see the poster and become familiar with the PEC Survey. Rostering for the PEC Survey takes place in early summer. The rosters that practices provide are submitted online through the PCF portal using a template. Health IT vendors can support practices in the creation of their patient rosters. More information about roster submissions will be distributed to practices and health IT vendors closer to the roster submission period. The CMS contractor will select the survey sample. The PEC Survey data collection begins in September and ends in December each year. Patient responses to the survey determine the practice score. This score is used to evaluate the practice's strengths and needs in providing patient centered care. Practice scores will be available in the PCF Portal in the spring. The survey vendor will be able to give survey results faster, before CMS’ PEC score report is available.